Health
Organ Transplant Waitlist Integrity Questioned Amid New Rules

The integrity of the organ transplant waitlist system in the United States is under scrutiny following investigations launched by the Trump administration. In September 2023, the government announced a review of state organ procurement organizations due to serious safety breaches, including attempts to remove organs from living patients. While these actions warrant investigation, the focus on isolated incidents diverts attention from a broader issue that threatens fairness in the transplant system.
Since the introduction of a new heart allocation system in 2018, practices that could be seen as manipulating the waitlist have become increasingly common. Developed by the nonprofit organization United Network for Organ Sharing (UNOS), the six-tier classification replaced an older three-tier system. This new structure aimed to more precisely assess patients’ urgency for transplantation based on their medical conditions. However, according to experts, the implementation of these rules has inadvertently incentivized questionable practices that undermine its original intent.
The revised system prioritizes patients in the top two tiers, aiming to expedite transplants for those in the most critical condition. Nevertheless, some doctors have begun utilizing aggressive treatments, such as surgically implanted heart pumps, to elevate their patients’ statuses on the waitlist. These practices raise ethical concerns, as they may push less-sick patients ahead of those who genuinely need immediate care.
A study published in Transplantation Direct in 2020 highlights this troubling trend. The use of intra-aortic balloon pumps among waitlisted patients skyrocketed from just 3% in 2017 to 45% after the new allocation system was implemented. This dramatic increase occurred without evidence suggesting that patients were any sicker than those treated prior to 2018. Additionally, mortality rates for patients with these pumps in Tier 2 were comparable to those treated with medications alone in Tier 3, indicating that the system may not accurately reflect disease severity.
The findings suggest that the current organ allocation framework encourages unnecessary invasive treatments, which can lead to complications and further exacerbate the challenges of equitable resource distribution. While the desire of physicians to secure transplants for their patients is understandable—given that approximately one-third of candidates die while waiting—the methods employed to achieve this goal can blur ethical lines.
The stakes are high with a limited supply of donor hearts; enhancing one patient’s status can disadvantage another. Reports from the field indicate that this culture of waitlist manipulation has become so pervasive that physicians feel compelled to escalate treatments to ensure their patients are not left behind. Furthermore, there are concerns that the financial incentives tied to increasing transplant volumes may also influence these practices, as more transplants result in increased funding and improved outcomes for medical facilities.
Recognizing the ethical dilemma, the transplant community must take steps to restore fairness in the organ allocation system. A crucial initial measure would involve standardizing the criteria for exception requests, ensuring consistency across all patients rather than favoring those at centers with more resources to advocate for them. Currently, exception status is granted to about 30% of waitlisted patients, significantly enhancing their chances of receiving a transplant.
Additionally, the processes by which regional boards evaluate these requests require scrutiny to prevent manipulation. A more effective solution could involve developing a new assessment system that determines medical urgency independently of the treatments administered by doctors. Some transplant specialists have been collaborating with UNOS to create a scoring system based on objective medical data, which has successfully reduced gaming in lung transplant allocations.
Despite these efforts, federal agencies have recently directed transplant organizations to halt progress on this initiative, opting instead to focus on investigating rare procurement errors. This decision risks prolonging the inequities currently present in the system. The prevalence of waitlist gaming poses a significant threat to the safety and fairness of the organ transplant process, impacting the lives of countless patients waiting for life-saving procedures.
As the transplant community grapples with these challenges, it is imperative to prioritize the development of a system that equitably assesses the medical urgency of patients, safeguarding the integrity of organ allocation for future generations.
-
 Science1 month ago
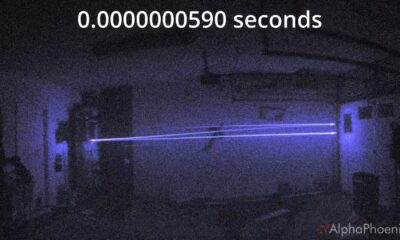
Science1 month agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 Top Stories1 month ago
Top Stories1 month agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Entertainment2 months ago
Entertainment2 months agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal









