Health
Effective Alternatives to Hormone Therapy for Menopause Relief

Managing menopausal symptoms can be challenging, particularly for women who cannot use hormone therapy. This is the case for Shilpa Gajarawala, a 58-year-old physician assistant from Jacksonville, Florida, who faced issues such as hot flashes, night sweats, and sleep disturbances due to her history of breast cancer. Gajarawala spent two years attempting to manage her symptoms without medical intervention. However, healthcare professionals emphasize that alternatives to hormone therapy exist, which can effectively alleviate these symptoms.
Recent updates to medication labels may lead to increased awareness of non-hormonal treatment options. Many women still rely on hormone therapy, but concerns about its side effects and contraindications have prompted some to seek alternative solutions. Conditions such as severe liver disease, prior heart attacks, strokes, blood clots, or hormone-sensitive types of breast cancer can limit the use of hormone therapy. According to Dr. Stephanie Faubion, medical director at the Menopause Society, “There’s always a solution. We have lots of other options available.”
Exploring Lifestyle Changes
Incorporating lifestyle changes can significantly impact the management of menopausal symptoms. While exercise may not directly alleviate symptoms, it helps with weight loss, which is linked to a reduction in hot flashes and night sweats. A combination of aerobic activities, such as walking or running, and strength training is recommended to maintain bone density.
Diet also plays a crucial role. Emerging research suggests that a “plant-forward diet,” which emphasizes fruits, vegetables, and soy while minimizing oil, can help manage hot flashes. Gajarawala has already made dietary adjustments, eliminating red wine and focusing on healthier foods. Doctors advise avoiding potential dietary triggers like caffeine and alcohol to further minimize symptoms.
Maintaining cardiovascular health becomes particularly important during menopause due to the decline in estrogen and progesterone production, which can lead to increased blood pressure and cholesterol levels. Dr. Faubion stresses the importance of lifestyle habits such as quitting smoking, ensuring adequate sleep, and managing stress to support heart health.
Non-Hormonal Prescription Options
In addition to lifestyle modifications, several non-hormonal prescription medications can help alleviate menopausal symptoms. Antidepressants, for example, have been shown to ease hot flashes and improve mood. Recent research indicates that oxybutynin, a drug typically prescribed for overactive bladder, may also reduce hot flashes while addressing frequent urination common during menopause.
New medications have entered the market, including Veozah, known as fezolinetant, which targets the brain region regulating body temperature. This drug blocks signals that trigger hot flashes and night sweats. Another medication, Lynkuet, has recently received approval from the U.S. Food and Drug Administration and works by blocking two specific molecules in the nervous system.
Despite these advancements, patients should be aware of potential side effects. The label for Veozah includes a warning regarding the risk of rare but serious liver injury. Lynkuet may cause fatigue and difficulty staying awake, while some antidepressants could lead to weight gain at higher doses. Dr. JoAnn Manson from Harvard Medical School notes, “There’s no medication out there that’s entirely free of risk.”
Additional Non-Hormonal Treatments
Women can also find relief through over-the-counter products. Vaginal lubricants can alleviate dryness, while cognitive behavioral therapy has shown effectiveness in helping women cope with hot flashes. Dr. Faubion points out that while such therapies may not eliminate hot flashes, they can reduce their perceived intensity and burden.
Moreover, clinical hypnosis has emerged as a promising option, with some studies indicating it may decrease the frequency and severity of hot flashes. Dr. Manson mentions that while more research is needed, the evidence thus far is encouraging.
The critical takeaway for women experiencing menopausal symptoms is that they do not have to endure them passively. Dr. Juliana Kling, a women’s health expert at the Mayo Clinic Alix School of Medicine, emphasizes the importance of discussing treatment options with healthcare providers. Gajarawala took this advice to heart by seeking alternatives that suited her needs, resulting in significant improvement in her quality of life.
Ultimately, as healthcare professionals continue to explore effective treatments and lifestyle modifications, women are encouraged to take charge of their health during menopause and seek out personalized solutions that work for them.
-
 Science4 weeks ago
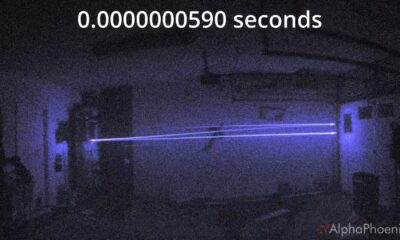
Science4 weeks agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health1 month ago
Health1 month agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories1 month ago
Top Stories1 month agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment1 month ago
Entertainment1 month agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Business1 month ago
Business1 month agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 Entertainment1 month ago
Entertainment1 month agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 World1 month ago
World1 month agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health1 month ago
Health1 month agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Entertainment1 month ago
Entertainment1 month agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal
-

 Health1 month ago
Health1 month agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Science1 month ago
Science1 month agoNorth Carolina’s Biotech Boom: Billions Invested in Manufacturing
-

 Top Stories1 month ago
Top Stories1 month agoDisney+ Launches Chilling Classic ‘Something Wicked’ Just in Time for October









