Science
New Biomarker Testing Approaches Revolutionize NSCLC Management

The approach to biomarker testing in non-small cell lung cancer (NSCLC) is evolving significantly, as new protein-based and computationally derived markers gain prominence. This shift is largely driven by the introduction of innovative therapies, particularly antibody-drug conjugates (ADCs), and a deeper understanding of therapeutic resistance and vulnerability. During the 20th Annual New York Lung Cancers Symposium on November 15, 2025, Dr. Soo-Ryum (Stewart) Yang, an assistant attending pathologist at the Memorial Sloan Kettering Cancer Center, highlighted several pivotal trends in this field.
Dr. Yang identified four key developments: the emergence of protein-based immunohistochemistry (IHC) biomarkers for ADCs, the growing actionability of tumor suppressor genes, the therapeutic potential of synthetic lethality, and advancements in computational pathology. The ongoing challenge of tissue scarcity underscores the urgent need to develop multiplex IHC methods and integrate broad panel next-generation sequencing (NGS) alongside artificial intelligence (AI) to enhance personalized therapies for a broader NSCLC patient base.
The traditional focus on a cancer cell’s genetic makeup is now complemented by the examination of protein expression levels on cell surfaces. This shift allows pathologists to identify actionable biomarkers that could unlock new treatment avenues. While PD-L1 IHC testing has been a staple for guiding checkpoint inhibitor therapy, its application is now extending to ADCs. Dr. Yang emphasized two critical protein biomarkers in NSCLC: HER2 and c-MET overexpression.
HER2 overexpression is present in up to 20% of NSCLC patients, with the highest IHC staining (3+) found in approximately 3% of cases. Notably, there is no direct correlation between HER2 mutation status and overexpression. Most NSCLC instances showing high-level gene amplification correspond to IHC 3+ staining, although not all 3+ cases result from amplification. The FDA recently approved fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) for HER2-positive solid tumors, including NSCLC patients who have undergone prior treatment. This approval was backed by the phase 2 DESTINY-Lung01 study, which utilized HER2 scoring guidelines initially developed for gastric cancer.
Similarly, c-MET overexpression is prevalent in NSCLC, with over 50% of tumor cells exhibiting 3+ staining found in up to 17% of EGFR wild-type cases. This biomarker can coexist with other driver mutations but is distinct from MET exon 14 skipping mutations and MET amplification. In May 2025, the FDA granted accelerated approval to telisotuzumab vedotin-tllv (teliso-V; Emrelis) for this patient demographic, backed by results from the phase 2 LUMINOSITY trial.
As Dr. Yang noted, integrating HER2 and c-MET IHC screening poses significant challenges to current diagnostic workflows. He proposed that institutions adopt flexible, standardized options allowing for optimized workflows tailored to their specific resources. Several promising biomarkers are currently under investigation, which could refine personalized treatment for NSCLC patients.
KRAS mutations, particularly the KRAS G12C variant, occur in up to 40% of lung adenocarcinomas. KRAS G12D mutations, associated with a history of little or no smoking, show a lower tumor mutational burden and PD-L1 expression, correlating with poorer responses to chemoimmunotherapy. Established therapies targeting KRAS G12C, such as sotorasib (Lumakras) and adagrasib (Krazati), are already in use. Additionally, clinical trials are underway for targeted therapies that extend beyond KRAS G12C, including multi-RAS inhibitors.
Dr. Yang highlighted the potential of zoldonrasib (RMC-9805), a KRAS G12D inhibitor, which demonstrated a promising overall response rate of 61% in a phase 1 study. The multi-RAS inhibitor daraxonrasib (RMC-6236) also shows potential in treating KRAS G12V-mutant NSCLC.
Mutations in tumor suppressor genes, specifically STK11 and KEAP1, are present in up to 20% of lung cancers and are often co-mutated with KRAS. These mutations can lead to an immunosuppressive tumor microenvironment and primary resistance to immunotherapy. Data from the phase 3 POSEIDON trial indicate that combining a CTLA-4 inhibitor with PD-L1 inhibitors and chemotherapy could enhance outcomes for these patients. This positions STK11/KEAP1 mutations as critical indicators for escalating checkpoint therapy strategies.
Detection of these mutations requires broad-panel NGS, as standard PCR methods are not suitable due to the complexity of inactivating mutations across these tumor suppressor genes. Dr. Yang also addressed the role of MTAP deletions, which occur in approximately 18% of lung cancers. These deletions create a metabolic vulnerability that can be targeted therapeutically, exploiting a “first hit” with a “second hit” strategy through PRMT5 or MAT2a inhibitors.
The quest for comprehensive biomarker testing continues, with TROP2 emerging as a target for ADC development. The phase 3 TROPION-Lung01 study examined datopotamab deruxtecan-dlnk (Dato-DXd; Datroway) as a second-line treatment, revealing a progression-free survival benefit over docetaxel. However, the study did not focus on a specific biomarker due to a lack of correlation between TROP2 expression and treatment response.
To enhance predictive power, researchers have developed an AI-driven method that measures TROP2 staining through computational pathology. This approach generates a quantitative continuous score, which when applied retrospectively, showed promise in predicting higher response rates.
Although these advancements are encouraging, Dr. Yang cautioned about the current reliance on a proprietary digital pathology ecosystem for TROP2 assessment, raising concerns about accessibility and broader implementation. He emphasized the need for a more holistic approach to lung cancer treatment that integrates protein analysis, AI insights, and novel therapies like synthetic lethality.
In conclusion, the landscape of NSCLC management is shifting dramatically, moving beyond traditional genomic focus to a comprehensive approach that includes advanced protein analysis and AI-driven methodologies. As these strategies develop, they promise to enhance personalized medicine for lung cancer patients, making it an increasingly accessible reality. Dr. Yang summarized the importance of exploring multiplex IHC and broad-panel NGS in the coming years, envisioning them as foundational elements of comprehensive biomarker testing in lung cancer.
-
 Science4 weeks ago
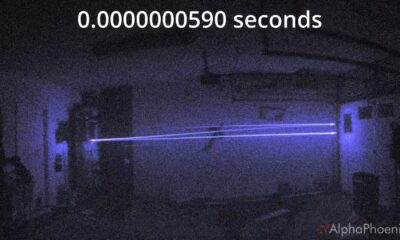
Science4 weeks agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health1 month ago
Health1 month agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories1 month ago
Top Stories1 month agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment1 month ago
Entertainment1 month agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Business1 month ago
Business1 month agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 Entertainment1 month ago
Entertainment1 month agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 World1 month ago
World1 month agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health1 month ago
Health1 month agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Entertainment1 month ago
Entertainment1 month agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal
-

 Health1 month ago
Health1 month agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Science1 month ago
Science1 month agoNorth Carolina’s Biotech Boom: Billions Invested in Manufacturing
-

 Top Stories1 month ago
Top Stories1 month agoDisney+ Launches Chilling Classic ‘Something Wicked’ Just in Time for October









