Health
ACIP Delays Hepatitis B Birth Dose Decision, Sparks Controversy
On September 19, 2023, the Advisory Committee on Immunization Practices (ACIP) postponed its vote on the hepatitis B birth dose, a long-standing vaccination protocol for American newborns. Since 1992, infants in the United States have received this vaccine at birth, but ACIP’s proposed change would delay the vaccination until at least one month of age. This decision has raised significant concerns among health professionals regarding its implications for public health.
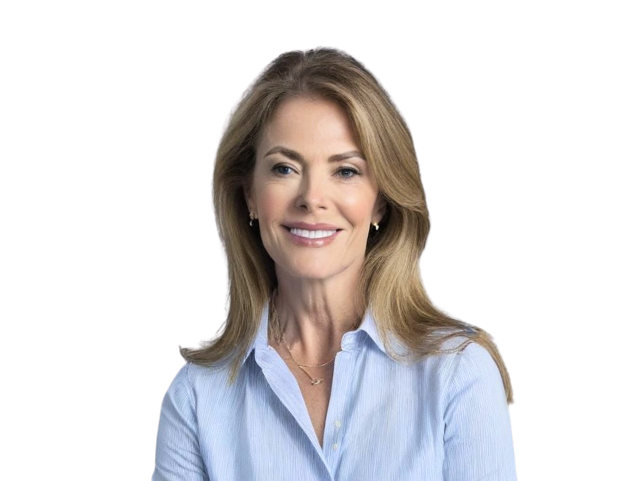
The current universal vaccination strategy aims to protect the small percentage of newborns at risk of perinatal hepatitis B infection, primarily linked to mothers with chronic hepatitis B. Monique Yohanan, MD, MPH, a senior fellow at Independent Women, argues that delaying the birth dose undermines the safety net for approximately 1% of infants who are vulnerable while continuing to expose 99% of infants without risk to potential vaccine adverse effects.
Yohanan highlights that the primary justification for the birth dose was to safeguard those few pregnancies at risk, estimated to be around 22,000 pregnant women with chronic hepatitis B in the early 1990s. Without intervention, approximately 6,000 of these women were at risk of transmitting the virus to their newborns. In contrast, current estimates suggest that around 18,000 infants are born each year to mothers positive for hepatitis B, with only about 200 developing chronic infections.
Flaws in Universal Vaccination Strategy
Yohanan contends that the assumption that a birth dose would confer lifelong immunity and protect against infections acquired later in life, particularly through intravenous drug use (IVDU), is misguided. Research indicates that antibodies from the vaccine diminish within 15 years for most recipients, leaving adults at risk without meaningful protection from early vaccinations.
The policy has been deemed successful in preventing chronic hepatitis B infections; however, it has also led to millions of unnecessary vaccinations for infants who are not at risk. The repercussions of this universal approach are evident, as families have received federal compensation for adverse effects resulting from the hepatitis B vaccine, including serious disabilities and deaths.
Yohanan criticizes the decision to delay the birth dose, stating that it fails to protect at-risk infants while still subjecting the majority of vaccinated children to unnecessary risks. She emphasizes that a more effective public health approach would focus on targeted vaccination strategies aligned with individual risk factors.
Proposed Solutions for Targeted Vaccination
To improve the current vaccination landscape, Yohanan advocates for a comprehensive strategy that addresses the root causes of hepatitis B infections in the United States. Key proposals include incorporating hepatitis B testing into immigration medical evaluations to identify infected family members and connect them to necessary care.
For women at risk due to IVDU, leveraging existing healthcare encounters can enhance identification and targeting for vaccination. Currently, women who use injection drugs often engage with healthcare systems during overdose or injury incidents. Expanding routine testing for hepatitis B during these encounters could better link vulnerable populations to preventive measures.
To ensure at-risk infants receive necessary vaccinations, hospitals should adopt a policy mandating that newborns receive hepatitis B immunoglobulin along with the vaccine if their mother is positive or if her status is unknown. Only a documented negative test from the current pregnancy should allow for exceptions to this rule.
Yohanan suggests that if universal vaccination is still considered, it may be more appropriate to shift it to adolescence, aligning vaccination with common healthcare touchpoints such as pre-high school visits. This shift would allow for discussions about risk factors and provide necessary protections as individuals enter vulnerable stages of life.
The hepatitis B vaccination policy established in 1992 was primarily a product of administrative convenience. In 2025, with advancements in data collection, technology, and healthcare infrastructure, there is an opportunity to refine the approach to better serve at-risk populations. Implementing real reform would involve protecting infants who are genuinely at risk, connecting mothers to appropriate care, and aligning vaccine timing with individual risk factors.
In conclusion, while the ACIP’s decision to delay the hepatitis B birth dose may seem like a step towards reform, it is, according to Yohanan, merely a postponement of necessary changes to a flawed system. Transitioning from a universal vaccination strategy to a targeted approach could lead to more effective public health outcomes and improved trust in vaccinations as a whole.
-
 Science1 month ago
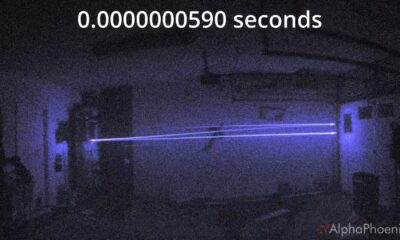
Science1 month agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
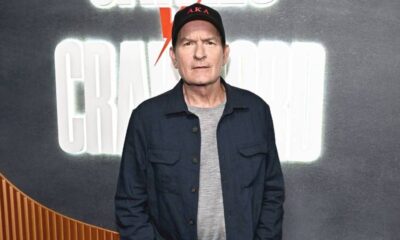
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 Top Stories1 month ago
Top Stories1 month agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Entertainment2 months ago
Entertainment2 months agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal









