Health
ACOs Urged to Expand Focus on Specialty Care for Cost Control

Recent insights from Theresa Hush, CEO and Co-founder of Roji Health Intelligence, highlight the urgent need for Accountable Care Organizations (ACOs) to broaden their focus beyond primary care. As the Centers for Medicare & Medicaid Services (CMS) shifts its emphasis towards cost control, ACOs must enhance their involvement in specialty care to achieve significant savings. The introduction of the Transforming Episode Accountability Model (TEAM) in January 2026 presents a vital opportunity for ACOs to adapt and thrive.
ACOs have traditionally concentrated on the management of chronic diseases such as diabetes and hypertension, primarily through primary care physicians. However, specialty services account for approximately 40 to 60 percent of total healthcare costs, indicating that a narrow focus could hinder long-term financial sustainability. As ACOs face an increased level of downside risk, integrating specialty care into their strategies will be essential for addressing escalating costs effectively.
To support this transition, CMS has introduced two payment models aimed at enhancing specialty care cost management: TEAM and the Ambulatory Specialty Model (ASM). These models are designed to provide ACOs with the necessary tools to leverage specialty services, thereby improving overall care quality and cost efficiency.
Understanding the TEAM Model
TEAM episodes are structured around five high-cost procedure types, including coronary artery bypass grafting (CABG) and lower extremity joint replacements. These episodes begin with the procedure and extend for 30 days post-operation, encompassing all Medicare Part A and B costs. A recent analysis by Roji Health Intelligence found that hospital inpatient and outpatient expenses represent the largest share of costs within these episodes.
Moreover, surgical complications significantly contribute to cost variability. For instance, complications can result in prolonged hospital stays and increased use of intensive care services. By reducing these complications, ACOs can significantly lower average costs associated with TEAM episodes.
A crucial factor in minimizing surgical complications lies in addressing patient risk factors prior to surgery. A lack of communication between primary care physicians and specialists can contribute to adverse outcomes. For example, a patient with a history of cardiac issues may encounter complications like atrial fibrillation following surgery if their risk factors are not adequately managed beforehand.
Strategic Recommendations for ACOs
To effectively participate in the TEAM model, ACOs should consider the following strategies:
1. **Serve as a Primary Care Referral Source**: ACOs can help patients without existing primary care relationships to obtain necessary assessments prior to surgery. This proactive approach ensures that surgeons and anesthesiologists have a comprehensive understanding of the patient’s health status.
2. **Establish a Communication Platform**: Effective communication is essential for the success of TEAM procedures. ACOs should develop a shared platform that allows primary care providers, surgeons, anesthesiologists, and other specialists to access patient risk information and treatment histories. This collaboration can facilitate advanced planning, including virtual consultations with anesthesiologists.
3. **Collaborate with Specialty Practices**: ACOs should partner with specialty practices to enhance data sharing and analytics capabilities. By aggregating clinical and cost data, ACOs can better assess episode costs and quality metrics. This collaborative approach is vital for meeting the requirements of the TEAM and ASM models.
The TEAM model represents an important shift in how ACOs must approach healthcare delivery, extending their responsibilities beyond traditional primary care management. As ACOs are expected to take a more active role in managing specialty care, the financial incentives provided by CMS aim to motivate organizations to enhance their care coordination efforts effectively.
With the implementation of TEAM and ASM, the healthcare landscape is poised for transformation. ACOs that embrace these changes will not only improve patient outcomes but also contribute to more sustainable healthcare spending. As the focus on specialty care intensifies, the time is ripe for ACOs to redefine their roles and responsibilities in the healthcare ecosystem.
Through these strategic initiatives, ACOs can position themselves to thrive in an evolving model of care that prioritizes both quality and cost-efficiency.
-
 Science4 weeks ago
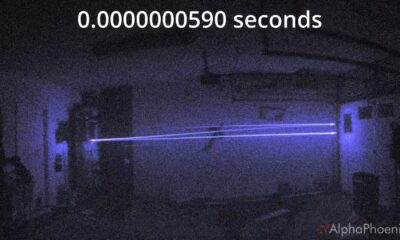
Science4 weeks agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health1 month ago
Health1 month agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories1 month ago
Top Stories1 month agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment1 month ago
Entertainment1 month agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Entertainment1 month ago
Entertainment1 month agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 Business1 month ago
Business1 month agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World1 month ago
World1 month agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health1 month ago
Health1 month agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Entertainment1 month ago
Entertainment1 month agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal
-

 Health1 month ago
Health1 month agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Science1 month ago
Science1 month agoNorth Carolina’s Biotech Boom: Billions Invested in Manufacturing
-

 Top Stories1 month ago
Top Stories1 month agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast









