Health
German Patient Achieves HIV Remission Through Unique Stem Cell Transplant

A significant breakthrough in HIV research has emerged as a 60-year-old man from Germany has achieved sustained remission from the virus following a stem cell transplant originally intended to treat leukemia. This case, detailed in a study published in Nature, represents the seventh documented instance of HIV remission through stem cell transplantation. What makes this case unique is that the donor cells contained only one copy of the CCR5-delta32 mutation, a departure from previous successful cases that required two copies.
The patient, who had lived with HIV for over a decade and was on antiretroviral therapy, underwent the transplant in 2015 after a diagnosis of acute myeloid leukemia. Six years after discontinuing his HIV medication, extensive testing revealed no detectable virus in his system, leading researchers to declare him functionally cured. Initially, the transplant aimed to save his life from cancer, not HIV, yet the outcome has generated considerable excitement in the medical community.
Potential for Broader Treatment Approaches
Researchers at Charité – Universitätsmedizin Berlin conducted thorough analyses, including biopsies and advanced sequencing, to confirm the absence of replication-competent HIV. This remission has persisted without any rebound of the virus, a challenge encountered by many experimental therapies.
Prior to this case, notable instances of HIV remission, such as that of Timothy Ray Brown—the first documented patient cured in 2008—relied on donors who were homozygous for the CCR5-delta32 mutation. This mutation renders cells resistant to most strains of HIV by blocking the virus’s entry into these cells. Although the cases of Brown and the so-called London Patient in 2019 set a high standard, the rarity of suitable donors limited the scalability of such treatments.
The new case, often referred to as the “next Berlin Patient,” suggests that donors who are heterozygous for this mutation, which are much more common, could potentially expand the options for treatment. This insight builds upon a trend where stem cell transplants are yielding cures for HIV in a small subset of patients who require them for blood cancers.
Exploring Gene Therapy and Future Implications
This discovery underscores the need for innovative approaches in HIV treatment, particularly since the transplant process has shown the ability to eradicate the HIV reservoir—latent viral hideouts that traditional antiretroviral therapies cannot eliminate. The International AIDS Society presented a report at the AIDS 2024 conference highlighting the necessity of finding alternatives to bone marrow transplantation, which remains a high-risk procedure with mortality rates around 30% due to complications such as infections and graft failure.
Medical experts on platforms like X have expressed optimism that this case could lead to more accessible treatment strategies, potentially democratizing cure options beyond the limited pool of homozygous donors. Some experts have suggested that this could inspire less invasive approaches to gene therapy, mimicking the effects of partial genetic resistance.
While the excitement around this case is palpable, researchers caution that stem cell transplants are not a feasible option for most HIV patients, who currently manage their condition effectively with daily medications. Consequently, there is a growing focus on developing “cure-in-a-box” solutions, such as injectable gene editors or latency-reversing agents capable of flushing out viral reservoirs.
The implications of this research extend to future clinical practices and funding initiatives aimed at developing scalable solutions for HIV. With the World Health Organization estimating over 39 million infections globally, the urgency for effective treatments is critical. The National Institutes of Health (NIH) is backing studies to further investigate these promising avenues.
As research continues, the case of the German patient—from his HIV diagnosis in 2005 to his leukemia treatment and subsequent remission—illustrates both the potential and the challenges in the quest for a definitive cure for HIV. While this case does not provide a universal solution, it paves the way for future innovations in treatment and highlights the importance of refining techniques to make them more accessible to a wider population. As the medical community reflects on this case, there is a collective hope that the lessons learned will contribute to a future where HIV remission is not an exception but a regular outcome.
-
 Science1 month ago
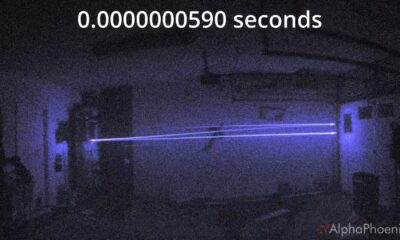
Science1 month agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 Top Stories2 months ago
Top Stories2 months agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Entertainment2 months ago
Entertainment2 months agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy









