Health
Global Health Crisis: Drug-Resistant Infections Surge Rapidly

A recent report from the World Health Organization (WHO) highlights a troubling escalation in antibiotic resistance, challenging a cornerstone of modern medicine. The findings reveal that in 2023, approximately 1 in 6 infections tested globally were resistant to antibiotic treatment. This alarming trend suggests that we are losing the battle against drug-resistant infections at a faster rate than previously anticipated.
Antibiotics have transformed deadly infections into manageable ailments and have made critical medical procedures, such as surgery and chemotherapy, safer. Yet, each use of these powerful medications carries a risk of fostering antibiotic resistance. Kevin Ikuta, an infectious disease physician at the University of California, Los Angeles, emphasizes that this phenomenon is a natural evolutionary process. He states, “We are in this battle we’re trying to lose as slowly as possible anytime we treat an infection.”
The WHO report indicates that nearly 40% of antibiotics prescribed for common infections, including urinary, gut, blood, and sexually transmitted infections, have diminished in effectiveness over the past five years. Ramanan Laxminarayan, president of the One Health Trust, expressed concern, noting, “We do see increases in resistance every year, but here we see a pretty sharp increase.”
The impact of antimicrobial resistance is already severe, directly causing about 1.2 million deaths annually and contributing to nearly 5 million more, according to WHO data. Laxminarayan warns, “We’re sleepwalking into a disaster,” highlighting the urgency of addressing this growing public health crisis.
Resistance Hotspots and Global Disparities
The increase in antibiotic resistance is most pronounced in low- and middle-income countries, where health systems are less equipped to manage infections. These regions often report higher rates of resistance, particularly for prevalent infections in tropical areas, where nearly 50 to 60% of cases may be drug-resistant. Laxminarayan explains that this disparity can stem from both biased data collection, which captures primarily severe cases, and genuinely higher resistance levels.
Inadequate healthcare infrastructure exacerbates the issue, as these countries typically lack robust infection prevention measures, vaccination programs, and effective water and sanitation systems. Furthermore, easy access to antibiotics without prescriptions contributes to misuse, such as inappropriately treating viral infections, which can exacerbate resistance.
While misuse is rampant in lower-income countries, the more pressing issue is that effective antibiotics, particularly those used in wealthier nations, are often unavailable to those who need them most. Laxminarayan points out that while patients in the United States can access alternative treatments if initial antibiotics fail, individuals in nations like Côte d’Ivoire or The Gambia may not have that option. This lack of access leads to insufficient treatment and further fuels antibiotic resistance.
Addressing the Growing Threat
The rising resistance rates of commonly prescribed antibiotics, particularly carbapenems and fluoroquinolones, are concerning. As these first-line treatments become less effective, healthcare providers are often left with older, more toxic options or newer medications that are not widely available. Ikuta notes, “So we’re either left with an untreatable infection or with a treatment where the side effects may be as toxic as the infection itself. It’s quite the pickle, clinically.”
To combat this crisis, a comprehensive understanding of global resistance patterns is essential. Although an increasing number of countries are sharing data with WHO, significant gaps remain. In 2022, nearly 48% of countries did not report any resistance data, and among those that did, many lacked robust surveillance systems.
Improving surveillance can help doctors make informed decisions about antibiotic use, leading to more effective treatments that can mitigate resistance. Additionally, there is a pressing need for the development of new antibiotics that target bacteria in innovative ways. Unfortunately, the global pipeline for new treatments is not advancing quickly enough to meet the growing demand.
Ikuta warns that if we fail to make progress, the medical advancements we often take for granted could be jeopardized. “It’s not just the treatment of acute infections and sepsis, it’s making sure surgery is safe and effective, and chemotherapy is available,” he explains. As antibiotics remain crucial to modern medicine, the ongoing loss of their effectiveness poses a significant threat to public health worldwide.
-
 Science2 months ago
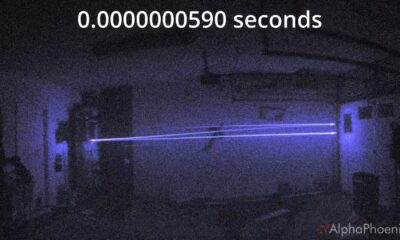
Science2 months agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Top Stories2 months ago
Top Stories2 months agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Entertainment2 months ago
Entertainment2 months agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal









