Health
Researchers Uncover Why Asthma Drugs Work for Some Kids, Not Others

Researchers at the Indiana University School of Medicine have made significant strides in understanding the varied responses of children to biologic treatments for asthma. Their recent study aims to identify which children are likely to experience severe asthma attacks despite being prescribed specialized medications. This research is crucial for enabling health care providers to intervene earlier and customize treatments based on individual needs.
Asthma is a prevalent chronic condition among children, affecting 4.6 million youths under 18 years old in the United States, according to the Centers for Disease Control and Prevention. The condition impacts lung function and can lead to symptoms such as wheezing, coughing, and shortness of breath. While effective monitoring and treatment can manage symptoms, poor management can result in severe flare-ups and life-threatening attacks.
Specialized medications, known as biologics, are often prescribed to target specific pathways in the immune system for children suffering from severe asthma. However, these therapies do not always yield the expected results. In a study published in the journal Pediatric Allergy and Immunology, researchers analyzed data from 122 children with moderate to severe asthma treated with biologics prescribed by pediatric pulmonologists and allergists affiliated with Indiana University Health. The goal was to uncover why some children respond better to these treatments than others.
“Our results demonstrate that, beyond a patient meeting existing guidelines for biologic treatment, routinely collected clinical parameters can help identify patients at an increased risk of severe asthma attacks,” said Arthur Owora, Ph.D., MPH, an associate professor of pediatrics at the IU School of Medicine and the study’s first author. This finding allows clinicians to adopt more proactive strategies to prevent exacerbations and manage health care costs effectively.
The study identified several clinical factors that influence treatment efficacy, including a child’s sex, age at treatment initiation, lung function, and white blood cell levels. Owora emphasized that their predictive model is a cost-effective and scalable solution that can identify children at higher risk for severe asthma attacks compared to existing methods. This is particularly beneficial for those who do not respond well to their initial treatments.
“Taking steps toward more personalized treatments that target the underlying causes of asthma specific to the patient leads to better outcomes,” Owora noted. “It’s important to ensure the right patient is matched with the right biologic, as not all patients respond to the same targeted drugs, and current generic prediction tools are not perfect.”
The research team is now focused on the next phase of their work, which involves providing these predictive tools to front-line clinicians and assessing their effectiveness in improving patient outcomes. The findings underscore the importance of tailored treatments in managing childhood asthma and highlight the ongoing need for research in this area.
The study, titled “Prognostic utility of pre‐biologic treatment correlates of childhood severe asthma exacerbation risk: Real world evidence,” is set to be published in Pediatric Allergy and Immunology in 2025, further contributing to the body of knowledge in pediatric asthma management.
-
 Science2 months ago
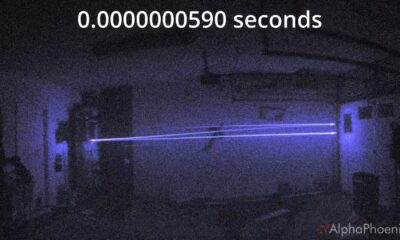
Science2 months agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Top Stories2 months ago
Top Stories2 months agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 Health2 months ago
Health2 months agoYouTube Launches New Mental Health Tools for Teen Users
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments









