Health
Young Users Face Rising Dangers of Cannabis Hyperemesis Syndrome

The emergence of cannabis hyperemesis syndrome (CHS) is leading to increasing hospital visits among young cannabis users, as evidenced by the experiences of individuals like Sydni Collins. At just 23 years old, Collins faced severe health challenges that culminated in multiple emergency room visits due to this debilitating condition, characterized by severe nausea and vomiting. Despite spending nearly a month in the hospital and relying on a feeding tube, she struggled to quit using cannabis.
Collins began using cannabis at the age of 16, often resorting to her weed pen even as she battled extreme nausea. One notable incident occurred during her senior spring break flight, where she experienced relentless vomiting. “There were some days when it lasted until noon and I would not go to school because of how bad it was,” she recalled. This pattern of symptoms is a hallmark of CHS, which has gained attention in recent years, particularly with the increasing number of cannabis users among young people. In 2023, more than 2.5 million teenagers in the United States, roughly one in ten, were identified as casual cannabis users.
As the incidents of CHS rise, both the World Health Organization and the Centers for Disease Control and Prevention have officially recognized the syndrome by adding diagnostic codes. Collins did not receive a diagnosis during her initial hospital visit; instead, she underwent seven ER visits in one month due to her worsening symptoms. This lack of awareness around CHS among healthcare providers often leads to misdiagnosis. Many patients are mistakenly told they are suffering from food poisoning or a stomach virus.
Understanding Cannabis Hyperemesis Syndrome
The specific cause of CHS remains unclear, but leading theories suggest that prolonged use of cannabis may overstimulate receptors in the endocannabinoid system, resulting in disrupted control over nausea and vomiting. Dr. Brian Kendall, an emergency medicine physician based in Charleston, South Carolina, explained that chronic exposure to THC can lead to desensitization of CB1 receptors in the brain and gut. “This leads to the whole system misfiring and causing hyperemesis,” he stated.
Collins initially sought relief through methods such as hot baths, which ultimately worsened her dehydration. She struggled to regain a healthy weight, as the condition made food unappealing. “I would chew on ice cubes, I would lick the salt off pretzel rods,” she shared. Unfortunately, her symptoms persisted, leading to further complications and prolonged hospital stays.
Another individual, Dan McGovern, experienced similar struggles. Initially misdiagnosed with gastroesophageal reflux disease (GERD), he was a regular user of potent cannabis concentrates during his teenage years. “I would start getting cold sweats. It just got even worse,” he recalled, describing his episodes of extreme nausea and vomiting. After consulting a gastroenterologist, he learned that his symptoms were linked to his cannabis use.
The Cycle of Use and Misdiagnosis
For both Collins and McGovern, the cycle of using cannabis to alleviate symptoms while simultaneously exacerbating those symptoms is a painful reality. “Both [smoking and hot showers] usually got rid of the nausea,” McGovern explained, highlighting the vicious cycle that many CHS sufferers face. Despite their diagnoses, both individuals continued to use cannabis, struggling to break free from the dependency.
Collins eventually quit cannabis for nine months after her initial hospitalization but returned to using it after being diagnosed with Crohn’s disease, another condition that can cause similar symptoms. “Getting diagnosed with that made me think that’s probably what [the original symptoms] were from and it wasn’t the weed,” she reflected. This type of misinterpretation is common among cannabis users, as CHS symptoms can strike intermittently, leading individuals to assume they are unrelated to their cannabis use.
Both Collins and McGovern have faced significant mental health challenges due to their conditions. McGovern noted feelings of anxiety and isolation during his severe episodes, stating, “Sometimes I would just be bedridden for days or weeks.” Despite the hardships, he continues to use cannabis, although he has switched to less potent forms and limits his consumption to nighttime.
Collins, on the other hand, felt overwhelmed by her experiences with CHS. After enduring ten days of continuous vomiting, she broke down emotionally, expressing feelings of humiliation and embarrassment about her cannabis use. “I also just felt embarrassed having to tell my whole family that I smoke,” she admitted. Ultimately, her last hospital stay prompted her to quit cannabis two years ago. “The only way to figure out if [my symptoms] were from weed is if I stopped,” she said. Since then, she has found support through an online CHS group and utilizes an app to track her progress in abstaining from cannabis.
The rise of cannabis hyperemesis syndrome highlights the pressing need for increased awareness and understanding among healthcare providers, particularly as cannabis use becomes more prevalent among young people. As the conversation continues, it remains imperative for users to recognize the potential risks associated with chronic cannabis consumption, particularly as the medical community works to better understand and address this complex condition.
-
 Science2 months ago
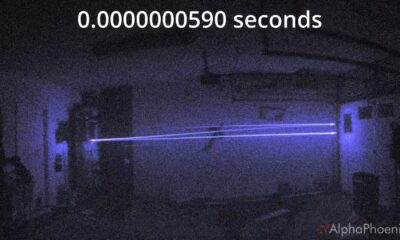
Science2 months agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Top Stories2 months ago
Top Stories2 months agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 Health2 months ago
Health2 months agoYouTube Launches New Mental Health Tools for Teen Users









