Science
Repurposed Drug Shows Promise in Reversing Alzheimer’s in Mice

Researchers at the University of Copenhagen have unveiled promising findings suggesting that a common amino acid, arginine, may reverse Alzheimer’s disease symptoms in mice. This discovery holds potential implications for millions affected by the neurodegenerative condition, which undermines memory and independence. The study indicates that arginine, often used to manage high blood pressure, may assist in clearing harmful brain plaques and restoring cognitive abilities in rodent models.
In the study, mice genetically modified to exhibit Alzheimer’s characteristics were administered arginine. These mice displayed the typical amyloid-beta plaques and tau tangles detrimental to neural communication. After treatment, the results were remarkable: the treated rodents showed reduced plaque accumulation and improved performance in memory tasks, such as maze navigation. Lead researcher Hans Christian Cederberg Helms noted that arginine enhances the brain’s waste-clearance mechanisms, potentially preventing toxic proteins from accumulating.
This research is not entirely unprecedented. Arginine has been previously studied for its benefits to vascular health. However, its application in neurodegenerative diseases represents a novel perspective. One significant advantage of arginine is its established safety profile; as a drug already approved for conditions like hypertension, it avoids many of the regulatory hurdles faced by new experimental treatments.
Implications for Alzheimer’s Treatment
The financial implications of repurposing existing drugs like arginine are substantial. New drug development often costs billions of dollars, making affordable alternatives attractive to pharmaceutical companies, especially those grappling with patent expirations and rising research and development pressures. The potential for quicker, less expensive pathways to human trials could attract significant investment into this area of research.
The mechanism underlying arginine’s effectiveness involves its interaction with the glymphatic system, which functions similarly to the lymphatic system but within the brain. In Alzheimer’s, this system becomes dysfunctional, leading to the accumulation of amyloid-beta. The Copenhagen team’s findings published in a peer-reviewed journal demonstrate that arginine enhances fluid movement through the glymphatic pathway, effectively “washing” the brain clean. Mice treated over several weeks not only exhibited fewer plaques but also showed behavioral improvements, including better social recognition and reduced anxiety-like symptoms.
While the results are encouraging, experts caution that findings in mouse models may not directly translate to humans. Past failures, such as anti-amyloid drugs that cleared plaques but did not prevent cognitive decline, highlight this gap. Despite these concerns, the low-risk nature of arginine makes it a strong candidate for rapid human trials, potentially within the next year.
Advancements in Nanotechnology
In parallel, advancements in nanotechnology have emerged as a transformative approach in addressing Alzheimer’s. Research teams in Spain and China have developed nanoparticles capable of crossing the blood-brain barrier, which poses a significant challenge for most therapeutic agents. According to a report featured in Medical News Today, these nanoparticles effectively reduced plaque levels by 50-60% in treated mice, resulting in notable memory recovery in various behavioral assessments.
This innovative approach employs magnetic nanoparticles that carry peptides designed to bind with and dissolve toxic aggregates. In one notable experiment published in 2025, mice receiving multiple injections over weeks experienced restored hippocampal function—the brain region essential for memory formation. This innovative delivery system enhances the precision of treatment, building on previous therapies that improved cognition in models of Down syndrome.
Pharmaceutical companies are closely monitoring these developments, as they could complement existing treatments like arginine. Major players in the industry, such as Roche, are investing heavily in this research area, with their experimental drug trontinemab slated for trials in late 2025. This drug aims to clear plaques through immunotherapy, and its potential synergy with nanotechnology or repurposed drugs could accelerate progress in a field desperately seeking breakthroughs.
The intersection of oncology and neurology also presents unexpected opportunities. Research from UCSF has shown that repurposed cancer drugs like letrozole and irinotecan can correct gene expression errors associated with Alzheimer’s pathology in mouse models. These drugs not only decrease plaque levels but also mitigate tau-related damage, enhancing motor skills and learning capabilities.
Despite the promise of these therapies, not all repurposing initiatives have proven successful. Trials from Novo Nordisk involving GLP-1 agonists, such as semaglutide, did not demonstrate benefits against Alzheimer’s in 2025, as reported by The New York Times. This setback has redirected interest towards vascular and amino acid-based therapies like arginine.
As excitement builds within the scientific community, social media platforms amplify these advancements. Posts detailing rapid plaque clearance in mice via nanoparticles have gained traction, further highlighting the potential for innovative treatments to emerge from ongoing research.
Future Directions and Ethical Considerations
Looking to the future, vaccines targeting Alzheimer’s present another exciting avenue. The Mayo Clinic is currently investigating vaccines designed to stimulate immune responses against amyloid-beta, with early studies indicating that vaccinated mice maintain cognitive function longer than unvaccinated counterparts.
While the potential for these therapies is significant, challenges remain. Differences in brain structure and disease progression between mice and humans contribute to high attrition rates in the transition from animal models to clinical application. Analysts estimate that only 10-20% of successful mouse studies translate into human approvals.
From a business perspective, repurposing drugs like arginine could disrupt the Alzheimer’s market, which is projected to grow at an annual rate of 18.7% through 2033, driven by an aging population. A report from OpenPR indicates that the availability of affordable treatment options could democratize access, particularly in underserved regions.
Ethical considerations also arise as the push for expedited trials intensifies. Ensuring diverse representation in clinical trials is critical, especially given that Alzheimer’s disproportionately affects older adults and minority populations. Recent research efforts have sought to incorporate genetic diversity in mouse studies, simulating broader human variability.
As these studies continue to evolve, the potential for achieving viable treatments for Alzheimer’s becomes increasingly tangible. The promising findings surrounding arginine, coupled with innovations in nanotechnology and repurposed cancer therapies, illustrate a multifaceted approach to combating this debilitating disease. As experts advocate for accelerated human trials, the insights gained from ongoing research may soon lead to therapies that can preserve cognitive function and improve quality of life for individuals affected by Alzheimer’s.
-
 Science1 month ago
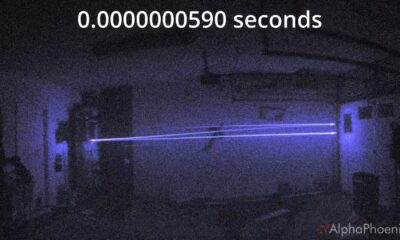
Science1 month agoInventor Achieves Breakthrough with 2 Billion FPS Laser Video
-

 Health2 months ago
Health2 months agoCommunity Unites for 7th Annual Into the Light Walk for Mental Health
-
 Top Stories2 months ago
Top Stories2 months agoCharlie Sheen’s New Romance: ‘Glowing’ with Younger Partner
-

 Entertainment2 months ago
Entertainment2 months agoDua Lipa Aces GCSE Spanish, Sparks Super Bowl Buzz with Fans
-

 Entertainment2 months ago
Entertainment2 months agoMother Fights to Reunite with Children After Kidnapping in New Drama
-

 Top Stories1 month ago
Top Stories1 month agoFormer Mozilla CMO Launches AI-Driven Cannabis Cocktail Brand Fast
-

 Health2 months ago
Health2 months agoCurium Group, PeptiDream, and PDRadiopharma Launch Key Cancer Trial
-

 Business2 months ago
Business2 months agoTyler Technologies Set to Reveal Q3 Earnings on October 22
-

 World2 months ago
World2 months agoIsrael Reopens Rafah Crossing After Hostage Remains Returned
-

 Health2 months ago
Health2 months agoNorth Carolina’s Biotech Boom: Billions in New Investments
-

 World2 months ago
World2 months agoR&B Icon D’Angelo Dies at 51, Leaving Lasting Legacy
-

 Entertainment2 months ago
Entertainment2 months agoRed Sox’s Bregman to Become Free Agent; Tigers Commit to Skubal








